Nurse depositions gone bad - part 1
Diagnosis and treatment - part 1 of 3
Introduction
Across the country medical malpractice litigation creates a painful scenario for the health care industry, causing incalculable financial losses and rendering emotional turmoil to the health care professionals who have been positioned unwittingly as pawns in the game. These pawns are often the ill-fated nurses who play a crucial role testifying in medical malpractice cases. Whether a seasoned nurse practitioner or a recently-employed CNA, the story is the same and it goes something like this:
A happily-employed, intelligent, and professional nurse receives notice of a deposition. Although she seems a bit anxious about having to testify, everyone believes “she will be fine” because she is smart, professional, and friendly. She has been instructed by counsel to keep her answers short, to “listen carefully to each question,” and to tell the truth. Unfortunately, what happens on deposition day (otherwise known as “D-Day” for the witness) is an all-too familiar picture experienced by defense attorneys, claims representatives, and nurses all over the country. Consider the following scenario:
Nurse Jones arrives for the deposition with some combination of the following feelings and emotions: anxiety, anger, frustration, apathy, fear, sadness, and even sympathy for the plaintiff. In spite of this, however, she is “ready” for her deposition because she has met with the lawyers and reviewed the medical records. The rest of the players arrive and take their places – plaintiff’s counsel is seated on one side of the table; defense counsel sits on the other; the court reporter gets situated; the videographer (often with a full A/V rig) sets up; and, much to the surprise of Nurse Jones, the plaintiff also arrives.
The stage is set. The shine of the videographer’s lamp illuminates the room. The camera is aimed at the witness. The court reporter swears in the deponent and the questions begin…. Despite Nurse Jones’ nervousness, things start out “OK” during the first few introductory and innocuous questions. Then it happens: a shift in the line of inquiry to the case specific questions, followed by a palpable change in the aura of the room. Tension increases, Nurse Jones’ anxiety elevates and before long, the nature and persistence of the interrogation has Nurse Jones doubting the quality of her nursing care. Slowly but methodically, Nurse Jones is led down a slippery slope on which she feels she has no choice but to “admit” that because the charting of the patient care in this case was “incomplete,” she, along with other nurses in the case, “breached the standard of care.” The next “admission” from Nurse Jones is that because she deviated from the exact wording of the hospital’s written policy, she must have again deviated from “the standard of care.”
Unfortunately, plaintiff’s counsel is just getting started. Much to the surprise of the defense team and co-defendants, Nurse Jones’ opinions do not stop with the nursing care; rather, she also responds to questions about the medical care and diagnoses of the patient. In due course, Nurse Jones even proffers opinions about the medical decisions made by the physicians and what they “should” or “should not” have done that “could have” or “would have” prevented the patient’s injury or death. At this point, defense counsel is white-knuckling his legal pad, and co-defense counsel is frustrated because his physician has just been “thrown under the bus” by Nurse Jones.
As if these admissions were not bad enough, during the course of the deposition, Nurse Jones’ anxiety causes her to make factual errors in her testimony. She becomes emotional (breaking down into tears), argumentative, angry, frustrated or perhaps even sarcastic with plaintiff’s counsel. This is all recorded in the permanent transcript of course, and the videographer also has it all captured and preserved on video. Defense counsel, stunned to say the least, now has to inform his client (the claims manager) about Nurse Jones’ catastrophic deposition.
The proverbial “bell has been rung” – loudly – and it will be re-rung by plaintiff’s counsel for settlement leverage, or as a way to provoke trial jurors. What should and could have been a relatively uneventful deposition, limiting plaintiff’s leverage and strengthening the defendant’s settlement position, has turned into a dream for the plaintiff’s lawyer and a nightmare for the defendants.
An emotional shift has taken place among all the parties involved in this case (see Table 1). The following quote from a Missouri-based medical malpractice defense attorney highlights the point: “Words can’t really do justice to describe the sick, sinking feeling that you get in the pit of your stomach when a key witness drops the ball at deposition in a case you know in your heart is otherwise defensible. It’s like getting punched in the gut when you aren’t expecting it.”
Table 1. Poor Deposition Emotional Effect
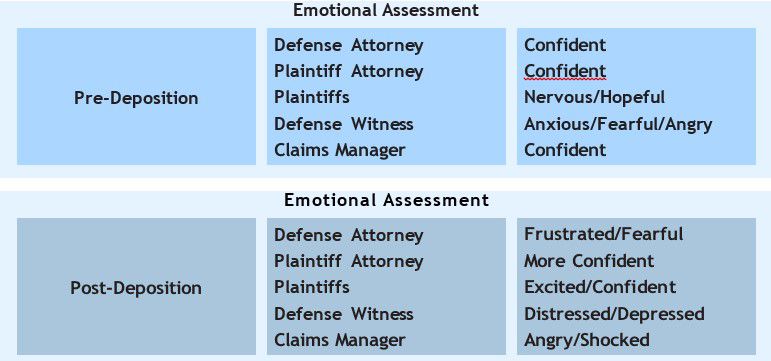
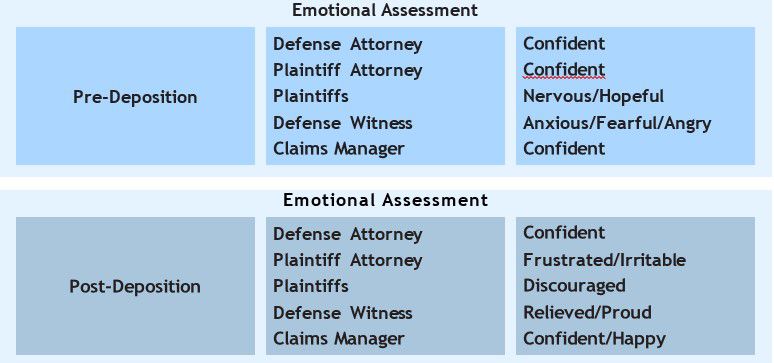
Table 2 below represents what would have been the result if the witness had been properly assessed and trained to testify effectively from both from the legal and the non-legal perspective. This quote from an Orlando-based medical malpractice defense attorney illustrates the point: “During the day, I watched my nurse respond warmly and positively to your advice as you built her confidence and communication ability. My nurse became convinced that your interests were her interests and became more and more able to incorporate the substantive points of the defense into her testimony as she worked with you. I believe the case is much stronger now than it would have been without your efforts.”
Table 2. Strong Deposition Emotional Effect
Deposition Post-mortem
A figurative “autopsy” must be performed by both defense counsel and the claims manager to determine the root cause of the disastrous deposition, which raises the following questions:
• Did Nurse Jones in the vignette really mean what she said?
• Does she harbor ill-will toward the hospital?
• Does she actually believe she and her nurse counterparts breached nursing standards of care?
• Does she really think she is qualified to offer medical opinions and that she had the right to criticize the clinical judgment of the physicians in the case?
If the answer to each of these questions is a resounding “NO,” then why did Nurse Jones testify as she did? Why did she …
Undermine the defense’s case?
Point the finger at the other nurses?
Admit to breaching multiple standards of care?
Criticize the medical judgment of the physicians?
Prevention cannot be addressed prior to causation and the answers to these questions can only be uncovered by first recognizing that the causes of a nurse’s struggle in the deposition are tied to certain aspects inherent to the profession as a whole. Many personality and job-related factors negatively impact nurses’ abilities to tell the truth effectively in a legal/adversarial context. These include the individual characteristics of the nurse in general; the nurse’s training (professional and academic); on-the-job experiences; the requirements and expectations from supervisors, physicians, patients, and patients’ family members; the pressures and demands of the job; and, additionally the strategic methods the nurse must employ to efficiently and effectively fulfill her various roles and responsibilities in the medical setting. Upon further analysis, it becomes clear that much of what it takes to make people GOOD nurses makes them POOR deponents, transforming one of health care’s greatest and valued assets into one of its biggest legal liabilities. Left unchecked, this leads to needlessly handing leverage and money over to the opposition.